SAN DIEGO COUNTY, Calif. —
Donovan Deaths
This is the first of a two-part investigation into how the prison system responded to the COVID-19 pandemic and what led to the deaths of 18 people at Donovan state prison in San Diego.
The crisis peaked four days before Christmas. San Diego’s only prison was teeming with COVID-19 infections. A fifth of the 3,500 people incarcerated were sick, and many were relocated to three large gymnasiums so staff could reach them quickly in an emergency.
Over the next five weeks, 18 inmates died from the virus.
Through county medical examiner reports, death certificates and interviews, inewsource pieced together how these people lost their lives to COVID-19 while under the care of the Richard J. Donovan Correctional Facility in Otay Mesa.
Three of the inmates were found unresponsive in their cells, inewsource has learned, despite the corrections department insisting that those with COVID-19 are regularly monitored and transferred to hospitals if they need more intense care.
The cellmate of one of the men who died, Gilbert Rodriguez, said the 66-year-old was denied medical treatment from prison staff after testing positive and coughing through the night. Prison officials refused to respond to specific questions about his Dec. 26 death.
“There is no crime that heinous that it sentences you to die of a virus and to not get medical attention,” said Hadar Aviram, a criminologist and professor at the UC Hastings College of Law in San Francisco.
Court filings indicate Donovan has among the worst track records of California’s 35 adult prisons in its response to the pandemic. The facility has acknowledged housing COVID-positive inmates with people who didn’t have the virus because the staff was overwhelmed by the winter outbreak. It was also the only prison out of compliance with court orders to create enough wheelchair-accessible beds in COVID-19 isolation areas when the surge in cases began.
The state’s prison oversight office found Donovan had issued its staff the most written citations in December of any prison for refusing to wear masks or practice social distancing. The prison is now tied for the third-most coronavirus deaths in the state.
The California Department of Corrections and Rehabilitation wouldn’t answer questions about individuals’ healthcare or deaths, citing medical privacy concerns. Marcus Pollard, the warden at Donovan prison, declined multiple interview requests through a spokesperson. The department only responded to questions from inewsource over email.
“We have worked tirelessly to implement measures in the face of a brand new virus and the
inherent constraints that exist with a critical 24/7 operation,” said Terri Hardy, a spokesperson for the state prison system.
Eight days
The three men found in their cells, all 65 or older with pre-existing medical conditions, died within eight days of each other. Five other Donovan prisoners died at hospitals during that time.
Donovan guards discovered Ronald Johnson unresponsive in his single cell on the night of Jan. 2. San Diego County medical examiner reports show he had recently been diagnosed with COVID-19.
Johnson was moved to a triage room as the guards attempted CPR and called 911. When the paramedics arrived, they couldn’t save him.
“Nobody should be dying alone in a cell,” said Rebecca Fielding-Miller, an assistant professor of public health at UC San Diego, after learning about inewsource’s findings.
“There’s a lot of things you can do to prevent that,” she added.
Fielding-Miller said prisons should use frequent monitoring and testing to identify those who need more serious medical care. Plus, reducing the number of people incarcerated has proven to be an effective prevention tool that has not been fully used, she said.


Statewide, thousands of incarcerated people have been released from California prisons ahead of schedule, but advocates have called on officials to do more. In October, a state appeals court demanded San Quentin State Prison in Marin County cut its population in half after more than 2,000 inmates became sick.
A corrections department spokesperson said prisoners with COVID-19 are screened twice a day by medical staff. But its healthcare guidelines say infected inmates may need more attention than that because their conditions can deteriorate quickly — especially for those with underlying conditions who are showing symptoms.
When Johnson died, he was 69 and had lung disease, hypertension and cirrhosis, medical examiner records show. The Vietnam War veteran also suffered from PTSD, paranoia, bipolar disorder and narcotics addiction, according to a transcript from his 2016 parole board hearing. He needed a walker to help with his mobility.
Johnson was incarcerated for a 1992 drunken-driving crash that killed four people in Fontana. He was scheduled for another parole hearing in February, less than two months after he died from COVID-19 inside the prison.


“This punishment is not in the California penal code,” Aviram said. “Not even for people that are sentenced to death. This is not fair. This is not the way to treat other human beings.”
Aviram said prison medical staff across the state have struggled to keep up with the number of COVID-19 infections, making it possible for their seriously ill patients’ conditions to worsen unattended.
“The kind of healthcare that you get in prison, it’s not really healthcare,” she said.
Gravely ill
Ryan Rodriguez was shocked when he got the news the day after Christmas from his brother, who said the prison had called to inform them of their father’s death. Rodriguez had spoken with his father about a week earlier.
Gilbert Rodriguez tested positive for COVID-19 at Donovan on Dec. 23, medical examiner records show. He died three days later.
The family asked for details about Gilbert’s condition in the days leading up to his death, but the prison wouldn’t elaborate.
“Was he ever seen by a doctor?” Ryan Rodriguez said. “Was he ever put on any kind of ventilation? Was he ever put on any kind of meds? None of those answers were given to us.”

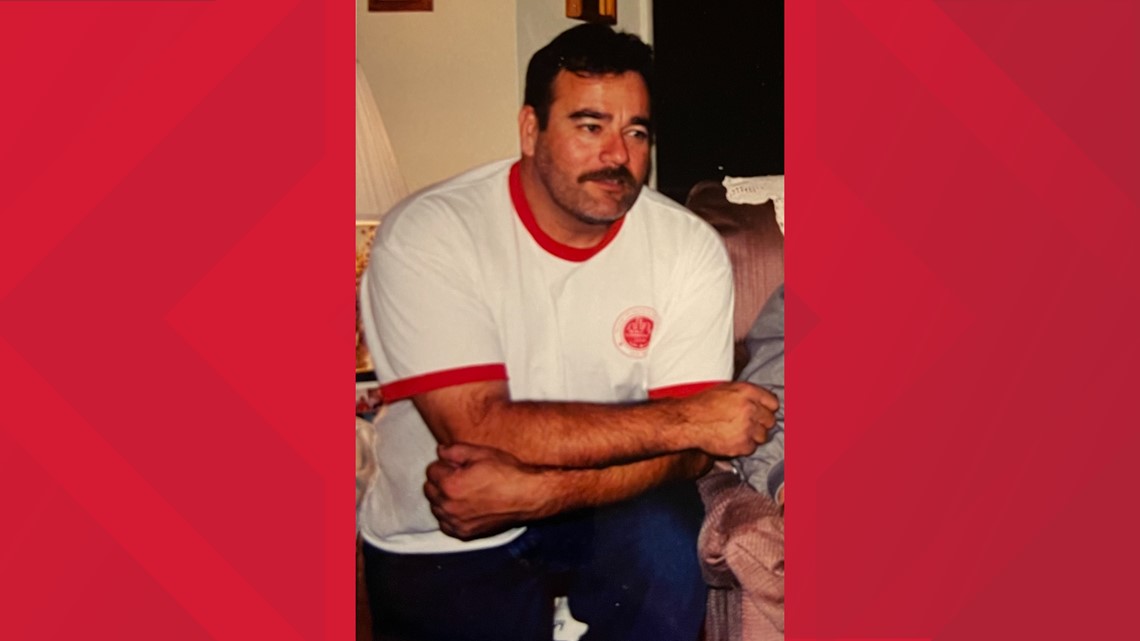
About a month later, he received a letter from his father’s cellmate, which said Gilbert had been coughing a lot after his diagnosis, and when he asked for medicine to soothe his throat, the staff did not give him any.
The coughing continued, the cellmate’s letter says, and Gilbert got almost no sleep two nights in a row. Then, he experienced what looked like symptoms of a heart attack or stroke, according to the letter, and died.
His dying wish was for his two sons to know about the lack of medical help available inside the prison, the letter says.
“I would expect anybody with underlying conditions getting COVID (to) be monitored and tracked at some level, not just left in a cell and say, ‘Good luck,’” Ryan Rodriguez said.
In March, Gilbert’s son received an email from the Medical Examiner’s Office with some of the only details he’s been told about his father’s illness. Healthcare staff made rounds and checked his father’s vitals every day, it said.
Medical records show Gilbert had diabetes and cardiovascular disease. He was also an addict who struggled at times with drugs and alcohol, his son said.
He was serving a life sentence with the possibility of parole for lewd and lascivious acts conducted with a child under 14.
People in prison are mostly there for a reason, his son said.
“I don’t expect them to be treated with white gloves, but I do feel like there should be something in place to address the situation when people become gravely ill,” Ryan Rodriguez said.
Susceptible to spread
Experts have noticed a troubling trend in California prisons — incarcerated people are refusing testing out of concerns they will be forced into isolation areas, which can be highly restrictive and similar to solitary confinement settings.
Penny Godbold, a San Francisco attorney who represents incarcerated people with disabilities, said her clients across the state have feared being transferred into isolation areas that don’t accommodate their needs.
“They were essentially trying to wait it out and get themselves better,” Godbold said.
In ongoing legal action against the prison system, Godbold’s firm claims Donovan guards have physically abused disabled inmates and then denied them medical care, leaving some too scared to seek help when they need it. About a quarter of people incarcerated at Donovan are disabled.
Godbold said her firm’s reports show about half of the 218 state prisoners who have died from COVID-19 had disabilities.
“These are serious red flags,” she said.
Kenneth Sandlin, a Donovan prisoner found dead in his cell, tested negative for the virus almost three weeks before his death, medical examiner records show. He refused to be tested again even after developing a persistent cough.
On Dec. 27, Sandlin told his cellmate he wasn’t feeling well and went to sleep on the top bunk. That afternoon, staff found the 65-year-old unresponsive and attempted CPR. They took him to the triage department, where he was pronounced dead.
The Medical Examiner’s Office tested Sandlin’s body and found he was positive for the virus.
Sandlin, who was serving a 25-year sentence for voluntary manslaughter, had cirrhosis, according to medical examiner records. That put him at an increased risk of complications from the coronavirus.


Incarcerated people have higher rates of many medical conditions, making them more susceptible to developing serious symptoms and dying from COVID-19. Prisons are also hotbeds for outbreaks because confined quarters and low airflow enable the virus to spread quickly.
The state corrections system began vaccinating inmates in December, but vaccines weren’t introduced at Donovan until after the worst of its outbreak had passed and inmates were already dead. As of this week, 73% of incarcerated people and 44% of staff are fully vaccinated. There is one active COVID-19 case.
Advocates say vaccinations in prisons are also essential to fighting the virus in the community. Research has linked high COVID-19 infection levels inside prisons to increased cases in neighboring areas.
Aviram, the UC Hastings law professor, said even though people imagine prisons as walled-off facilities, they operate more like membranes, with staff, volunteers and inmates leaving and entering each day. The activity puts the surrounding neighborhoods at risk.
“All of this enormous effort that everybody’s been putting forth in the last year, social distancing and masking and doing without and sacrificing,” she said, “all of this stuff is going to be worthless if we continue to incubate this disease in a place where hundreds of people go in and out on a regular basis.”
inewsource intern Kate Sequeira contributed to this story.
inewsource is a nonprofit, independently funded newsroom that produces impactful investigative and accountability journalism in San Diego County. Learn more at inewsource.org.
WATCH: California prisons see spike in COVID-19 outbreaks