SAN DIEGO COUNTY, Calif. — This story was produced as part of a collaboration with USA TODAY.
When Christine Russell read the message from the San Diego VA announcing it would no longer pay for her cancer treatment, all the pain came rushing back.
For nearly three years, the federally funded veterans' health care system had misdiagnosed her breast cancer as mental illness, she and her team of advocates contend. After discovering the cancer in late 2018 — when the tumors had already spread — the VA agreed to pay for the former Navy Reserve lieutenant to get her medical care from other doctors in the San Diego area.
Russell filed four federal complaints in early February this year about her ongoing challenges accessing health care, medication and caregiver services through the VA. Days later, a group of San Diego VA administrators mailed her a letter that called her “disruptive” and announced they would no longer fund her appointments outside the VA because her health care was too “fragmented.”
Russell was $30,000 in debt from medical expenses since developing cancer. She couldn’t afford to see her doctors if the VA didn’t pay for it.
“It was like they cut my legs off,” Russell said. “They cut off my lifelines, because all those doctors are my integrative support team. They are why I’m still alive.”


An inewsource investigation in partnership with USA TODAY has found that like Russell, veterans across the country are caught in the crossfire of the VA’s battle to retain patients and funding since the passage of a landmark health care law known as the Mission Act.
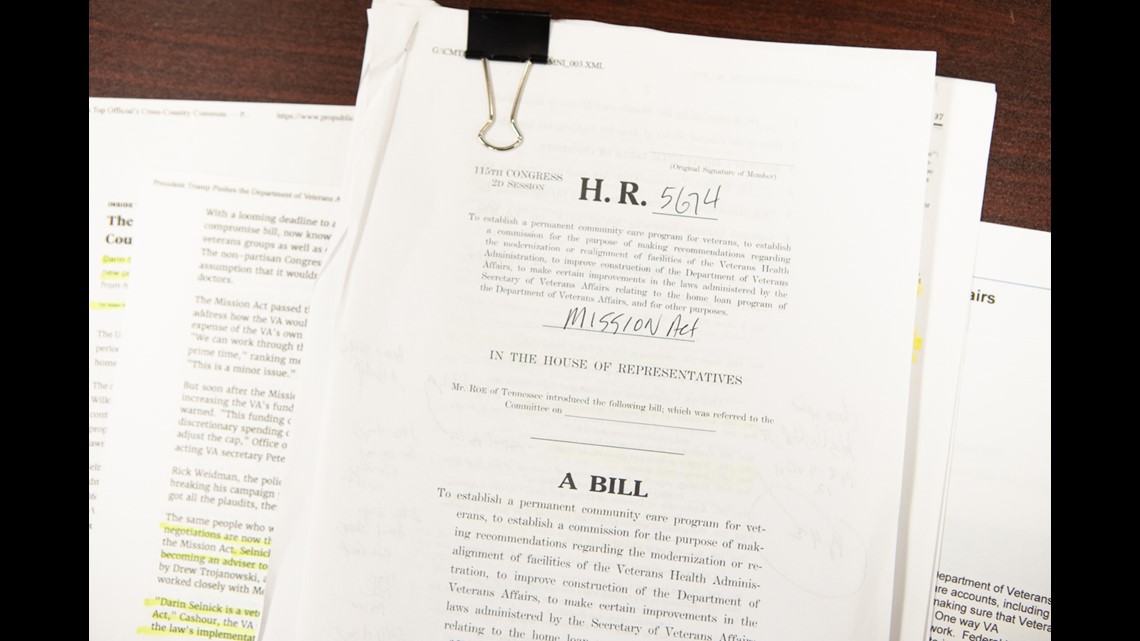
When Congress and then-President Donald Trump passed the bipartisan law in 2018, they said it would ensure American citizens who fight to protect the U.S. can access high quality medical care after leaving the military. When the Department of Veterans Affairs can’t deliver that care for any of six reasons, it’s supposed to pay other health care systems to do it instead.
A review of thousands of pages of department manuals and medical records, along with interviews with dozens of patients, advocates and providers, shows that VA administrators are overruling doctors’ judgments and preventing them from sending their patients outside the VA health care system.
This bureaucratic process has ramped up over the past two years as part of an effort to save money and retain patients within the VA, records show.
“That’s tragic and jarring,” said Ryan Gallucci, a national director for Veterans of Foreign Wars, after learning what the VA’s manuals show.
“I think it warrants an organization like ours asking more pointed questions and ensuring the VA is upholding the intent of the Mission Act,” he added.
More than 9 million veterans are enrolled in the VA, the nation’s largest health care system, which is composed of more than 170 medical centers and 1,000 outpatient offices.
The U.S. is facing urgent demands from veterans for medical and mental health care. Veterans have faced almost 20 million cancelled or delayed health care appointments during the COVID-19 pandemic, and the U.S. withdrawal from Afghanistan in August has caused crisis hotline calls to spike as former service members have struggled to process the unfolding events.
Dozens of veterans and caregivers throughout Southern California described their struggles to access health care outside the VA since the Mission Act was passed: A partially blind skin cancer survivor was told to take a dangerous trip to the VA when a new lesion developed, instead of visiting his neighborhood dermatologist. A veteran with a seizure condition has waited years for a course of treatment outside the VA. Suicidal patients were cut off from what they considered “life-saving” mental health treatments by employees overwhelmed with paperwork — against the advice of the VA’s own psychiatrists.
In interviews, service groups and Congress people from both political parties said veterans should be offered the best health care available, and money should not affect the quality of care they receive.
“We just spent trillions of dollars prosecuting this 20-year war in Afghanistan, and by comparison we’re arguing nickels and dimes in caring for the veterans who prosecuted those wars,” Gallucci said.
The Mission Act has had financial consequences for the VA. Since the law was enacted, more veterans have left for other health care systems than the VA anticipated, forcing the government agency to shell out billions of dollars for private care. If the trend continues, the VA’s own hospitals could end up with smaller budgets to spend on their services and staff.

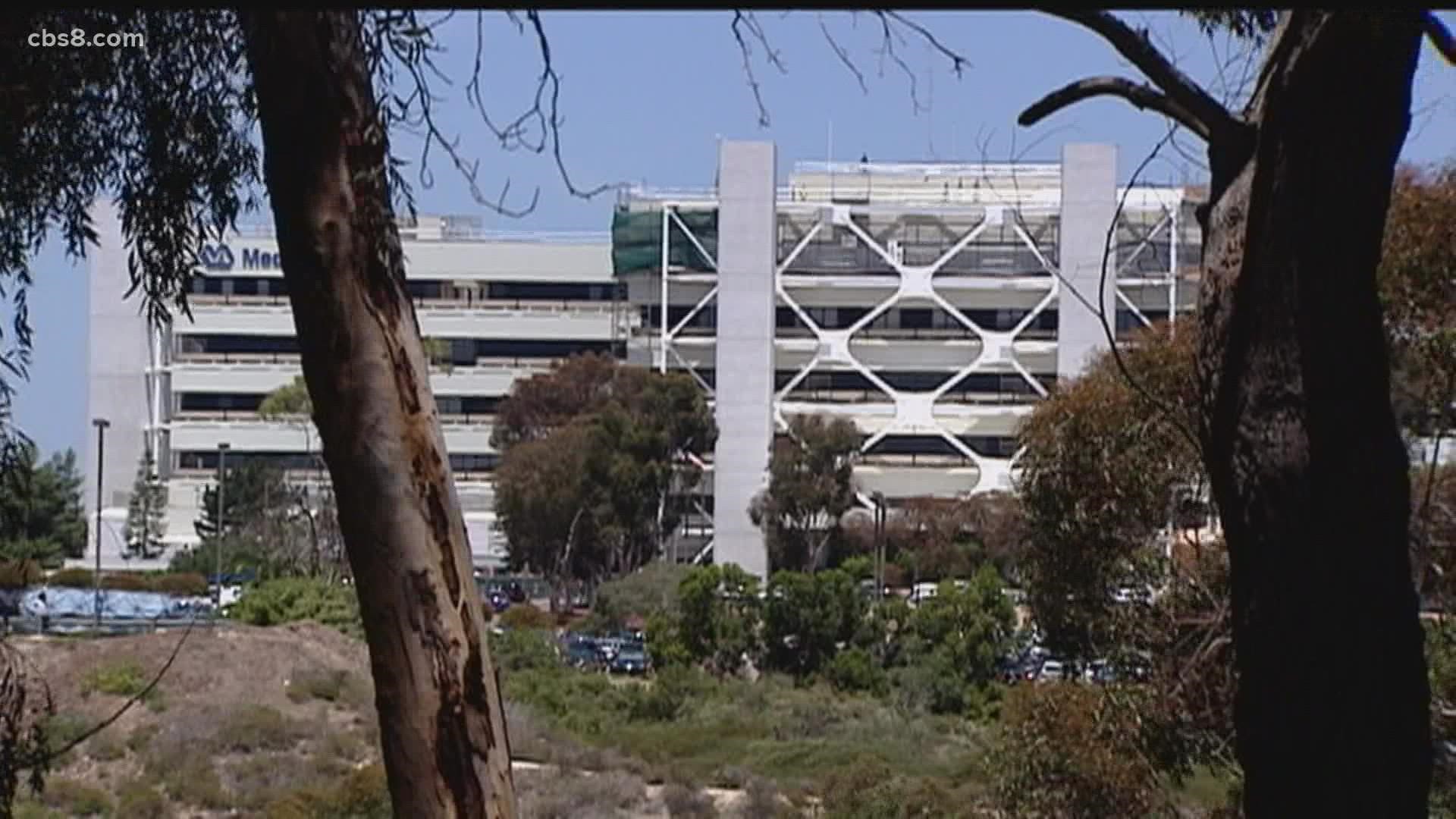
In late 2019, the VA began the “referral coordination initiative” to return veterans to its hospitals. An internal department manual shows the changes are supposed to help the VA make “good financial decisions” and “maintain funding of specialty care” in the future.
Like the VA, private health care systems have financial incentives to retain patients and cut costs. The difference, experts said, is that veterans represent a unique and vulnerable population that the government has pledged to care for.
“If they have a problem with the budget, they need to come and talk to Congress,” said Rep. Mike Bost, R-IL, ranking member of the House Committee on Veterans’ Affairs. “They don’t need to go ahead and try to figure out how to take services away from our veterans.”
Under department policy, VA doctors usually don’t send their patients outside the health care system on their own, records show. They can make recommendations that go through reviews by other staff — such as administrators, clerical workers or clinicians trained by hospital leadership — who can cancel treatment requests and insist patients come to the VA instead.
WATCH: The VA is Overruling Doctors' Medical Decisions Caption: An investigation by inewsource in partnership with USA TODAY has found that VA administrators are preventing doctors from sending their patients outside the VA health care system. Animation by Jorge Contreras
Following the VA’s new initiative, department hospitals have also set up select teams of health care personnel who can review medical records and use algorithms to decide if patients qualify for care outside the VA before interacting with those patients.
And for veterans ultimately approved for treatments elsewhere, the VA can require checkups at its hospitals anyway — that includes veterans facing severe disabilities, burdensome drives or long wait times for VA appointments.
“It basically defeats the whole purpose of the Mission Act,” said Darin Selnick, senior advisor to Concerned Veterans for America, an organization pushing for veterans to have more access to private health care.
“We need to be veteran centric,” he added. “It's about what the patient needs, not what the VA needs.”

Selnick helped write the Mission Act, working in the Trump administration and the VA as a health care policy expert to implement the law until July 2020. He read excerpts of the department manuals obtained by inewsource.
“If I was still at the VA and someone showed me this in July, I would have ripped it to shreds and I would have said there’s no way in Hell you’re going to use this stuff,” Selnick said.
The VA received its largest-ever budget this year — an amount that has doubled over the past decade. A national spokesperson said the department has “sufficient funds” to send veterans out for private care.
VA officials said they are following Mission Act requirements, and treatment decisions are based on patients’ medical needs. They added that the review process is supposed to ensure veterans can always get their care at the VA if they want to.
Hospital doctors and managers at the VA said they believe they can deliver the most effective care internally, because they offer high-quality services and can more easily coordinate treatments and paperwork.
Dr. Kathleen Kim, the San Diego VA chief of staff, said physicians sometimes incorrectly try to relocate patients for treatments her hospital can offer, and administrators are “regularly educating” them to help keep veterans at the VA.
“Because of the nature of the Mission Act, the VA is sending a lot of care in the community, and frankly we're worried that we're not going to be able to pay our bills,” Kim said.
The VA has approved over 12 million referrals for outsourced care since the Mission Act was implemented, including 5 million in the most recent 12-month period, according to data the department supplied. inewsource, through a series of records requests and direct inquiries, attempted to determine how many doctors’ requests for outsourced care have been denied by the VA, but the data provided was incomplete.
An August inspector general report highlights the personal impact the VA’s administrative decisions can have. When the San Diego VA stopped paying for ketamine treatments at a private clinic, 28 mentally ill patients experienced unnecessary distress, the report found. Inspectors pointed out the drug’s unique properties for combating severe depression.
Shortly after learning the VA wouldn’t fund her treatments, a former Marine Corps pilot took her life.


“They need to do right by these veterans,” said Rainelle Wolfe, a full-time caregiver for her husband Kiowa, another veteran who was cut off from the private ketamine treatments over a year ago.
The San Diego VA has started offering a low-dose version of the drug that many veterans have not found therapeutic, including Kiowa Wolfe.
Now, the Marine Corps veteran spends most of his time lingering in bed, reliving trauma from the Afghanistan War.
“We’re not political,” he said. “It’s not in our nature to be political. But keep politics and all this BS out of veterans’ health.”
Part I: A body on fire
Long before anyone realized she had cancer, Christine Russell walked slowly and painfully to the car waiting for her outside the San Diego VA emergency room. Her body hurt so much she could barely move.
The Lyft driver came out to assist her, then approached a nurse at the hospital entrance to ask if Russell would need any special care during her transport home. As the driver would later retell in a court filing, the nurse assured him the answer was no. The 39-year-old Navy veteran was “crazy” and imagining her symptoms.
It was mid-2018, almost two years since Russell first felt the unbearable pain in her body. It had become too difficult to drive or take care of herself, so she started paying thousands of dollars out-of-pocket for caregivers to look after her.
In her medical chart from late 2016, Russell’s VA physician wrote that she “displays abnormal anxiety about her health, especially with an unwarranted fear of having a serious disease.”
Russell said doctors told her she had post-traumatic stress disorder and refused to run tests until she tried psychotropic medications. Without a clear explanation for her escalating symptoms, Russell rushed to the emergency room more than a dozen times.
Finally, in the summer of 2018, her new primary care doctor agreed to order a scan of her chest. A radiologist noticed something unusual and asked for more tests.
The diagnosis: stage IV breast cancer.
Her case was complex. Russell suffers from severe allergies and sensitivities, which she believes came from her exposure to hazardous chemicals on a counter bioterrorism mission in the Middle East. Perfumes, highly processed foods and a long list of medications can aggravate her symptoms.


The VA’s course of cancer treatment, chemotherapy pills, was excruciating.
“It felt like my whole body was burning and on fire,” Russell said.
The veteran was also experiencing hormone imbalances and pelvis pain, which needed tailored treatments that wouldn’t cause their own unbearable side effects. Russell thought she would be better off getting care from specialists elsewhere — doctors she could trust who could better address her complicated symptoms.
Over the next three years, the VA approved a slew of requests for Russell to see at least eight specialists outside the department.
Her symptoms slowly improved. But traveling to her appointments was impossible without the help of an at-home caregiver. The VA tried to provide her with aides, but they didn’t follow the protocols Russell required for her sensitive immune system.
Russell hasn’t been able to get a new caregiver since November 2020, the same month she was supposed to begin radiation therapy. With no aide to assist her, the veteran never got the treatment.


Months of correspondence with VA employees didn’t resolve the issue. In February, Russell filed complaints with the VA’s inspector general and the White House.
That’s when she lost it all.
In a three-page letter, VA administrators told Russell they would no longer pay for her health care outside the department and insisted she follow the “code of conduct” moving forward. They said she had engaged in “disruptive behavior” by intimidating social work staff with angry voicemails, using profanity and telling them they should be fired for not doing their jobs.
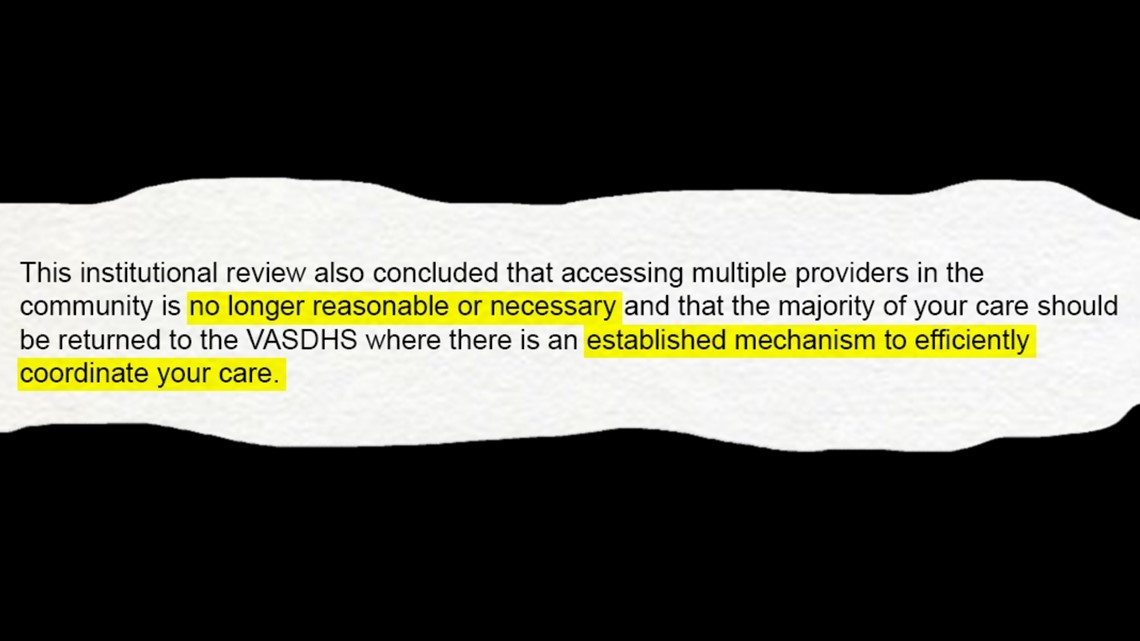
“The multidisciplinary team reviewed your current status and confirmed that your health care is
fragmented due to a disproportionate amount of care received in the community,” the letter states.
The administrators said this care was “no longer reasonable or necessary” and would be “limited to services that cannot be provided in a timely manner or are unavailable” at the San Diego VA, “as required by” national policy.

The letter was signed on Feb. 19 by the director of the Veterans Experience Office, the section chief of primary care and the chair of the Disruptive Behavior Committee.
Russell was not consulted about her health care needs before the letter was sent.
“It was a nightmare,” Russell said, adding, “They really didn’t know me or what I had gone through or why I was even still alive.”
She described her reaction as a “heavy mental breakdown” as she struggled with thoughts of suicide and almost checked herself into a hospital for psychiatric care.
If you are having thoughts of suicide, you can call the National Suicide Prevention Lifeline at (800) 273-8255 or the San Diego Access and Crisis Line at (888) 724-7240. Other resources are available here.
But she chose to argue her case instead.
Russell had done it before. When enrolled in the Navy, she filed a complaint about entry fees for military parties, which led officials to relieve her of her duties, escorting her out of Kuwait by military police. She then filed a whistleblower retaliation case, which was substantiated a year later by the Pentagon inspector general’s office.
“I’m always about integrity,” Russell said. “And if I see something that’s not ethical going on or if I see an error, because of what I’ve been through, I’m going to question that error.”
Part II: A veteran’s best interest
Armed with a copy of the Mission Act and her long clinical history, Russell told the San Diego VA that it was in her best interest to continue her medical treatments elsewhere.
The federal health care system will pay for veterans to get medical care from other doctors if the patients meet any of six criteria, including long drives or wait times for VA appointments.
The most contentious — and some argue, most critical — reason to send veterans outside the VA is when it’s in their “best medical interest.” That decision should be made by the veteran and their “referring clinician,” the law says, and can help address a patient’s unique needs.
Share your VA experience
inewsource wants to hear from veterans, caregivers and others who have interacted with the VA health care system. Tell us about your experiences with the VA by filling out this form.
For instance, a dermatologist might not specialize in a patient’s skin condition, or a veteran suffering from military trauma could be triggered by trips to the VA. In these kinds of cases, if it would improve a patient’s health, a doctor could send them to another medical provider.
“Every patient experiences things differently,” Russell said. “And if they’re not getting all their needs met, then it is in their best medical interest to go somewhere else to have all their needs met.”
Russell told the VA that stopping her current treatments would exacerbate her cancer symptoms — and it would put her health care back in the hands of a hospital that didn’t have the expertise for her conditions.
Her VA primary care doctor requested she return to her medical team outside the hospital, the veteran said, but warned the request probably wouldn’t be approved.


At the San Diego VA, these kinds of treatment requests are usually reviewed by “delegated authorities” who can deny them if they think the hospital’s own doctors can deliver the care.
Kim, the hospital’s chief of staff, said these designated physicians go through regular training, so they understand all the services the VA offers and can make more informed decisions than other doctors.
“Some of it, in my mind, is just a lack of knowledge about what the services are,” Kim said.
San Diego County is home to roughly a quarter million veterans, the fifth-highest of any county in the nation. Its local VA health care system, which also covers the neighboring Imperial County, serves about 85,000 patients.
Kim, who oversees veterans' health care across the region, said it’s often best for patients to come to the VA, even if that’s not what their doctors want.
“The reality is that does not trump the fact that the service can be provided at the VA within a timely fashion,” Kim added.


For a complicated case, Kim and leaders at other VA hospitals can personally review medical records and decide what’s in a patient's best interest, documents show.
The VA’s many hospitals can rely on different procedures, but nationwide, employees are instructed to follow handbooks. VA spokespeople were hesitant about providing them, saying they were intended for internal use.
Over the past two years, the VA has started putting treatment requests in the hands of “referral coordination teams” made up of registered nurses and other personnel, according to the manuals. A team member is supposed to spend 10 to 25 minutes reviewing a patient’s medical charts and deciding if they qualify for care outside the VA. They can also forward requests to designated physicians for approval.
The initiative “shifts the referral responsibility” so most doctors aren’t choosing to relocate their patients themselves, the documents show, which will “decrease inconsistent and inappropriate” treatment plans.
Hospital leaders are told to monitor health care costs as a “key performance indicator” of success.
“That is not what the Mission Act says,” said Rep. Bost of Illinois about the review process.
“I understand my health care and my doctor understands my health care,” he added. “Between the two of us, we make the decision, not some (team) that’s put in place by some government agency, nor should it be.”
The National VA pointed to federal regulations stating it can conduct reviews of doctors’ decisions so long as they focus on health outcomes. Spokespeople also said that VA doctors still have the power to send their patients outside their hospitals.
To do that, doctors have to use a specific software program that offers a pre-established list of justifications — otherwise it’s not considered a “true” medical decision, according to department manuals.
Once veterans are approved for care outside the VA, staff are supposed to call them and try persuading them to come to the VA anyway.
Employees are told to follow scripted language that outlines the benefits of staying at its hospitals and the burdens of leaving them. The scripts tell veterans they will be responsible for transferring their own medical records if they choose a different provider.
“If you wanted to stay in the VA, you always can stay in the VA, but once you’ve made a decision to go to community care, you’ve decided for whatever reason it’s best for you not to,” said Selnick, who helped write the Mission Act.


“Doing extra hoops to keep you in the system is counterproductive.”
When the VA stopped authorizing her treatments, Russell was left with two bad choices: pay out-of-pocket or stop seeing the doctors that had helped her through a complex cancer. She chose the expensive option.
With her credit cards maxed out, the veteran began an online fundraiser for the accumulating bills and turned to her church community for food deliveries.
The cancer has worn on her. Russell, now 44 years old, wakes up disoriented and forgets where she is. It takes her hours to clamber out of bed, and she inches forward around her house with the aid of a cane.
When she manages to leave her home, Russell adorns her outfits with American flags and, with a smile, tells anyone who will listen that she is proud to be an American. She still remembers the enthusiasm she felt 25 years ago as a teenager in Barstow, California, enrolling in the Naval Academy.


Through months of heated conversations, Russell was able to reestablish most of her old doctors.
But maintaining her care outside the VA is an ongoing problem. In August, Russell received a voicemail from her VA primary care doctor’s office. The physician had requested more appointments with specialists outside the hospital, and the requests were denied.
Russell is still searching for solutions.
Part III: Living with demons
The mental health crisis among America’s veterans can be told through a bleak series of statistics.
One in five veterans who served in Iraq and Afghanistan suffers from depression or PTSD, and more than half of veterans who need mental health treatments don’t receive them. About 17 former service members take their lives every day — double the rate of the general public — and the vast majority of veterans who died by suicide never sought services from the VA health care system.
Recognizing the troubling trend, the government has boosted its focus on mental health in the past few years. The VA has expanded its resources for suicide prevention, and Congress has put forward numerous bills to help address the issue.
But the VA can’t always provide the mental health support veterans need. Under the Mission Act, veterans have the same treatment rights for physical and mental health issues. If a patient isn’t benefiting from the VA’s services, their doctor can try to send them somewhere else.
That doctor, however, might not have the final say.
At the San Diego VA, administrative staff dismissed the warnings of psychiatrists and denied community mental health treatments to suicidal patients, records show. Soon after learning the treatments had been discontinued, one of the veterans died by suicide.
Over two and a half years, the San Diego VA sent more than 60 veterans to a private clinic to try the drug ketamine, a therapy for people with severe, treatment-resistant depression. Many of the patients showed remarkable improvements, and VA psychiatrists continued sending them back for sessions.
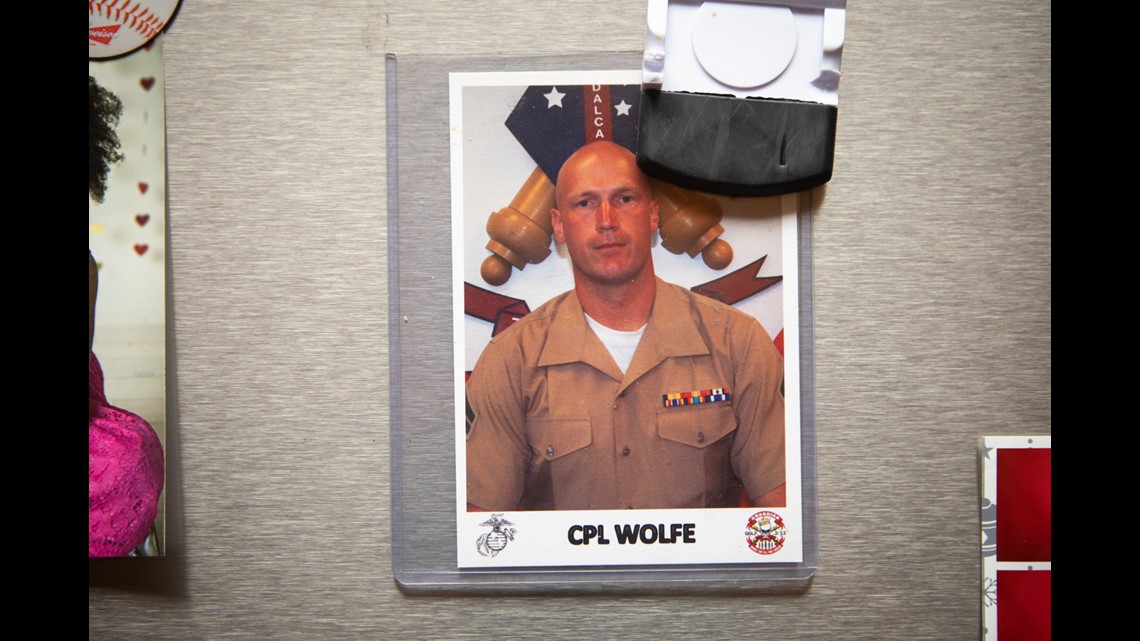
One of them was Kiowa Wolfe, a 38-year-old Afghanistan War veteran who was medically retired in 2018.


Nine years ago, Wolfe was defending a dam on a mountaintop in the Helmand Province when he took enemy fire. In the commotion, he stood up to get his bearings, and his 6’5” frame was instantly visible. Bullets flew in his direction and sent him tumbling down the side of the mountain.
The Marine returned from war with traumatic brain injury and wounds along his right side that demanded multiple surgeries. But his mental anguish hurt just as much. Intrusive memories of the battle overwhelmed him, and some days he felt he no longer wanted to live.
The VA classified him as 100% disabled, mostly due to his post-traumatic stress.
The government tried more than a dozen treatments, including a variety of medications and therapists. Nothing made a difference. Finally, Wolfe’s psychiatrist recommended ketamine. The VA didn’t offer it, so it paid for him to go to Kadima Neuropsychiatry Institute, a private clinic down the street.
Wolfe felt relief for the first time in years. He managed to walk into a movie theater and take his children to a Blink-182 concert — the kinds of activities he had once avoided at all costs.
“It cut down on the hyper-vigilence, where I’m not just freaking out and my head’s on a swivel everywhere, and I have to check out everybody and everything,” Wolfe said. “I could just actually relax and put my arm around my son and talk to him and act like a human.”
The drug’s effect typically lasts a few days. With the VA’s support, Wolfe returned for treatments twice a week, his wife always by his side.


That changed in October 2019, when a note appeared in Wolfe’s medical record from the VA Office of Community Care, which helps veterans arrange external medical appointments.
Dr. Susan Trompeter, the former chief of the San Diego office, issued a directive about the mentally ill patients on ketamine therapy. She called the drug “experimental,” said the VA could no longer pay for it and told the hospital’s psychiatrists not to submit any more treatment requests.
Trompeter, whose research focus is women’s reproductive health, did not respond to interview requests.
The VA Chief of Psychiatry pushed back, arguing the hospital could not “precipitously stop these treatments” for patients with severe depression. But the decision had been made, and he relayed the message to mental health staff.
“So please do not discuss/offer this as a possibility to patients until further notice from me,” Dr. Brian Martis wrote in an email. He told them not to “make verbal comments to patients or written comments… expressing your frustration” about the change.
Medical records and emails show VA doctors feared the sudden decision could be dangerous for their unstable patients. One veteran with a history of suicide attempts was a particular concern.
“We need to ensure he does not have a break in treatment,” one VA doctor wrote in his medical chart. Another warned of the “potential acuity of the situation” and said nobody had followed up with the veteran.
“I am concerned as this is a HIGH RISK pt,” the doctor added.
Under the Mission Act, patients are allowed to continue treatments outside the VA if they have ongoing sessions, because cutting them off can have negative consequences.
Kadima’s founder, Dr. David Feifel, decided veterans could keep their upcoming appointments even if the VA wouldn’t pay for them. He did it, he said, because he feared what would happen otherwise.


“Something’s out there that can help you, and now they’re taking it away,” Feifel said. “To have it and then not be allowed to have it makes living with those issues and demons even more difficult.”
After she learned the VA would no longer pay for her ketamine therapy, Navy and Marine Corps veteran Jodi Maroney died by suicide. inewsource first reported the death last year, prompting an investigation by the VA inspector general’s office.
In an August report, inspectors found the San Diego VA’s denial of care was a “contributory stressor” leading up to her death. But the circumstances were “multifactorial” and “complex,” the report said, and they couldn’t conclude the VA was responsible.
Hospital staff said they faced a “large volume” of referrals when the Mission Act went into effect in mid-2019, according to the report. The health care system needed to sign a new contract to pay for ketamine therapy, but the situation “was overlooked” until the VA missed its deadline.
For three weeks, the VA had no way to pay for ketamine therapy and didn’t explain to veterans why they couldn’t get their treatments. When Maroney died, the hospital quickly signed off on more sessions.
That lasted about five months. Starting in March 2020, the VA stopped paying for veterans to get ketamine therapy, even though the hospital’s psychiatrists had requested additional treatments.
For Wolfe, the VA’s decision was tantamount to betrayal.
“It feels like I’m getting stabbed in the back with a bowie knife and getting it twisted,” Wolfe said.
“If I was held to such high standards in the Marine Corps, why are these people getting away with so much with mistreating veterans?” he added.

Patients pleaded with hospital officials, describing how the drug had saved their lives, and shared suicidal thoughts and dreams with the private ketamine clinic.
Feifel sent frantic messages to VA psychiatrists and administrators, warning of a possible second death if the hospital didn’t act quickly.
“We were under the impression that the VA learned from its mistake and under no circumstance would it follow the same catastrophic path that resulted in that tragic outcome,” Feifel wrote. “And yet, here we are, watching a train wreck in slow motion… AGAIN!”
The VA never replied.
In an interview and emails, San Diego VA administrators have made multiple inaccurate statements about their ketamine program and health care services.
The hospital has repeatedly stated that community care staff don’t make clinical judgments and can’t overrule doctors — they process paperwork and help veterans set up appointments outside the VA.
Later, national VA spokespeople clarified that these employees do have the ability to review referrals, ask questions about patients’ clinical needs and cancel requests if they “cannot verify the eligibility” of the veterans.
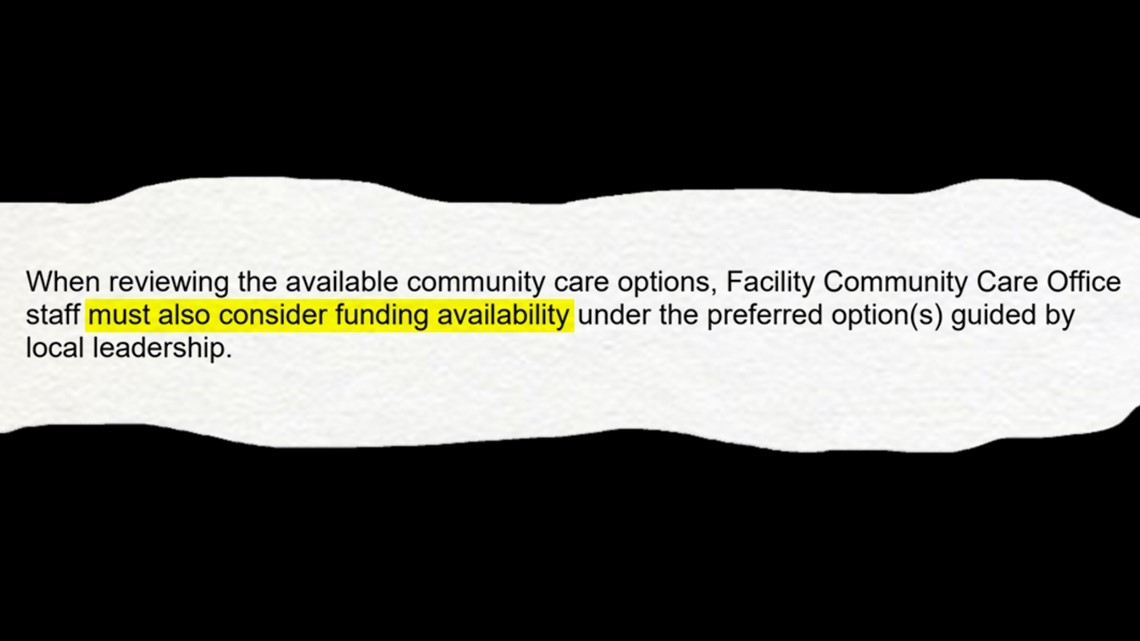
In VA manuals, community care staff are also instructed to “consider funding availability” when offering treatment options to patients.

In mid-October, the VA announced it will be phasing out community care offices over the next year and restructuring their responsibilities in order to “operate as a high-reliability, veteran-centric organization.” The VA has not explained if the transition will change how staff process treatment requests.
According to the inspector general report, San Diego’s community care employees chose to cut patients off from ketamine therapy the second time because of “administrative factors,” like outdated forms and misplaced paperwork.
The employees had “resistance to clinical input from mental health leaders” and caused serious distress to mentally ill patients, the report states.
Following the inspection, the San Diego VA hired more administrative staff and assured investigators they would base their decisions on veterans’ medical needs.
Those needs, as Wolfe would later find out, are up for interpretation.
Part IV: Circling the drain
Wolfe laid in bed, crippled by the memories that had resurfaced since the U.S. withdrew its last troops from Afghanistan.
All he wanted was a moment of relief. But the one treatment he knew would help was the one the VA wouldn’t pay for.
At $300 per visit, Wolfe can’t afford to pay out-of-pocket for regular ketamine therapy. Private donors have funded some sessions, and in times of crisis, the veteran has shelled out the full cost himself.
Wolfe and his wife Rainelle, who serves as his full-time caregiver, have spent the past year begging the VA to send him back to Kadima for more treatments.


“I do not have the ability to refer Kiowa to Kadima,” Wolfe’s VA psychiatrist wrote in a December message. “I am not involved in any way here at the VA with the implementation or adjudication of any aspect of the Mission Act.”
Medical records show Wolfe’s psychiatrist referred patients to ketamine therapy in 2018 and 2019, before the Mission Act went into effect.
“I know you are both suffering and wish you only health and happiness in the year to come,” the doctor wrote.
The hospital has refused to tell the Wolfe family who has the power to approve his treatment requests. VA doctors have told the veteran these are “administrative decisions” and they don’t know who’s responsible for making them.
“If you get the answers, call me,” one physician told Wolfe.
San Diego VA spokespeople would not give inewsource the names of the hospital leaders in charge of mental health treatment requests or provide a reason they wouldn’t share the information.
“If they’re not making the decision and not telling you who’s making the decision, how can you even advocate for the veteran?” said Renee St.Clair, Wolfe’s advocate and former chief operating officer at Kadima.
Veterans have avenues to fight the VA’s health care decisions, but attempting to use them can be a full time job. St.Clair, an attorney, is assisting the family pro bono. She has asked for help from more than a dozen service groups and government officials, including Congressional offices and the VA inspector general.


She also sends weekly emails to VA doctors and administrators asking them to approve Wolfe’s ketamine treatments.
“Kiowa gave so much and is asking so little—a signature on a form which could save his life,” St.Clair wrote in one message.
Veterans can submit clinical appeals to a VA hospital’s patient advocate’s office, which should be reviewed in three days by administrators, and then a second appeal that goes to regional VA leaders.
But veterans and caregivers who tried contacting patient advocates said staff either didn’t return their calls or didn’t help resolve their issues. The Wolfe family has not gotten responses from the San Diego office, they said.
How to appeal your case
Read the VA’s full clinical appeals process here. You can follow inewsource’s guide to navigating the VA’s health care decisions here.
The VA has never sent Wolfe a written denial of his treatment requests, like its policies describe.
“This is madness,” Rainelle Wolfe said. “I cannot believe that everybody’s acting like their hands are tied and they’re all passing the buck. Nobody wants to stand up and have some integrity and treat veterans the way they need to be treated.”
Since the San Diego VA stopped paying for his private sessions in mid-2020, Wolfe has been shuffled through the hospital’s attempts to build its own ketamine program. The ordeal has had disastrous consequences.
Over the course of two months, the VA administered different kinds of the drug at low doses. It didn’t work. Wolfe started backsliding into severe depression. But when the private clinic asked the VA to send him back for more appointments, a registered nurse in the local community care office denied the request.
It was “not clinically appropriate,” she wrote. The VA could provide the treatments he needed.
Then, in October 2020, VA nurses administered ketamine to Wolfe on a gurney in the post-anesthesia care unit. The family recalls that the veteran’s psychiatrist wasn’t present for the infusions, and he wasn’t allowed to bring his wife or service dog with him.
The experience was traumatic. Wolfe blacked out and entered a fit of rage. He screamed uncontrollably at his wife. When he finally got his bearings, he knew one thing absolutely. He would not come to the VA for another ketamine treatment.
Because of ketamine’s psychedelic properties, the drug’s effects are highly context-dependent. Changing how the drug is administered or delivering it to a patient in an uncomfortable environment could lead to negative outcomes.
Four veterans said the VA’s program has failed to provide the relief they need.
By personally paying for treatments and obtaining donor funds, St.Clair has helped nine patients return to Kadima for more ketamine sessions. She said at least twelve veterans have not found the VA’s program therapeutic.
Wolfe’s psychiatrist — considered the San Diego VA’s “local expert” on ketamine — has acknowledged to the veteran that the hospital’s program is “not the same” as what the private clinic offers.


Despite his towering height, Wolfe speaks softly and slowly, and he leaves most of the talking to his wife and four children. Their home is decorated with military memorabilia, the fridge featuring an old photo of the family patriarch in uniform. Rainelle, who met Wolfe in 2006 when he was 22 years old, has spent much of the past year rousing him out of bed, sometimes unsuccessfully.
“Is it really in his best interest to get all his care at the VA?” Rainelle Wolfe said. “Because he’s slowly circling the drain. He spends the majority of his time in his room in the dark.”
Asked why the VA won’t fund private treatments for veterans failing out of the hospital’s program, the chief of staff said it was a legal matter.
“The relationship with that clinic has become highly contentious,” Kim said. “And one of the former administrators every Friday sends what I would call a nasty email complaining about this issue. And so at this point, we’ve turned it over to legal counsel.”
In May, the Wolfe family had a brief moment of hope. Congressman Darrell Issa’s office convinced the hospital to take another look at the veteran’s case.
The VA conducted a “comprehensive review” of his medical needs, according to an email the Congressional office sent the Wolfe family.
The hospital “is confident that it is in your best medical interest to receive your mental health care (there) so that there is a comprehensive and integrated approach to maximize your treatment outcome,” it said.
The review was performed by an unnamed group of VA employees.
Part V: Closer to perfection
The Mission Act was passed in the midst of a fierce political debate over the future of the VA health care system.
The dispute dates back to 2014, when an overwhelmed VA hospital in Phoenix was caught concealing appointment wait times. The scandal prompted new laws and rules that let veterans access private care more easily.
But navigating health care choices was still a confusing and complex process, and Congress was looking for solutions. Democrats pushed to strengthen the VA with more funding and services, while Republicans wanted to make it easier for veterans to go to private doctors.
The Mission Act was their compromise. It created a network of approved community providers and expanded the reasons veterans could visit them. It also funnelled billions of dollars into the VA so the department could cover the expenses.

Now, veterans can get their primary and mental health care outside the VA if an appointment would take longer than a 20-day wait or 30-minute drive. For specialty care, that extends to a 28-day wait or a 60-minute drive.
“The Mission Act created an environment where all veterans, no matter where they live, would have access to VA care,” said Rep. Jack Bergman, R-MI, who voted for the law in 2018. “It may not necessarily be at a VA hospital, but at a place close to them where they can actually receive the care in a timely manner.”
But Southern California veterans said they are still struggling to get appointments with private doctors since the law was passed.
Former service members in rural areas — facing drives of an hour or more for VA visits — said they are routinely told to visit the department’s hospitals to assess whether care is necessary. Veterans facing long wait times said their private care can be cut off after a handful of sessions, and they have to return to VA physicians.
“It’s not working here,” former Army captain Gary Shearer said. “It hasn’t been working for some time.”
Shearer suffers from chronic neck pain and has gone blind in one eye, making each trek to the VA a dangerous burden. He lives in Yucca Valley, almost 50 miles from his VA primary care doctor and 80 miles from the closest veterans hospital.
Because of the long drives, Shearer qualifies for private doctor’s visits closer to home. But the VA has asked him to return to its own offices for checkups and assessments.
In December, Shearer saw a bump on his forehead that he knew needed medical attention. The veteran has a 20-year history of skin cancer and had cancerous lesions removed in the past. He wanted the Loma Linda VA to help him schedule an appointment with his neighborhood dermatologist.


The VA said no.
An “approving official” at the hospital reviewed his case, documents show. They decided a VA primary care doctor would have to conduct a skin exam first.
Shearer worried it would take months to go through this circuitous process: schedule an appointment at the VA, endure a long road trip for the visit, convince the doctor to request a dermatology appointment and wait for the VA to approve and schedule the request.
“The longer I waited, the more tissue they were going to have to take,” Shearer said.
The veteran didn’t want to take any chances, so he went to the dermatologist on his own. Shearer’s lesion was diagnosed as basal cell carcinoma and required an urgent surgery with a price tag of $3,000. It was too steep for him to pay out of pocket, but he was able to use his private insurance plan to cover the cost.
About one-quarter of working-age veterans — more than 730,000 people — don’t have a second medical payment option like Shearer does. If he didn’t have a backup insurance plan, the veteran said, he would have to rely on the VA’s medical decisions.
Shearer has a long list of grievances against the federal health care system. The VA cut down his weekly neighborhood chiropractor visits to only 12 sessions per year, despite his severe spinal injury from a military tank accident.
The back pain feels like “someone has taken a ball bat and beat me around the rib cage,” the veteran wrote in a complaint to the VA.
Shearer said he waited more than 50 days for an answer from the Loma Linda VA about extending his chiropractor appointments. The facility told him it could award up to eight more sessions per year if he agreed to drive all the way to the hospital for a pain assessment.
The former Army captain has sent many letters, ripe with colorful turns of phrase and religious proverbs, to the VA’s patient advocates. They led nowhere.
“The Mission Act, you say,” he wrote in one complaint. “What Mission Act? It is only a dream.”
VA manuals say veterans can receive an unlimited number of outsourced treatments, but only if reviewers deem them “clinically appropriate.”
Dr. Peter Kaboli, a VA physician in Iowa and health care administration expert, said having the department conduct reviews — and encouraging patients to come to the VA when possible — is better for veterans and the future of the health care system.
“Is there going to be an incentive to bring care back to the VA?” Kaboli said. “I think so, because I think we do it cheaper in most cases, and we do it as good if not better in most cases.”
Patients described their anguish when they have suddenly faced denials of care and letters demanding they return to veterans hospitals. Some said they have waited months or years for the VA to set up or renew appointments with private doctors.
WATCH: Waiting for VA health care - Former Navy combat engineer John Seymour and his wife Amy Warix recount their difficulties getting medical care through the VA health care system. Video by Zoë Meyers/inewsource
Patients described their anguish when they have suddenly faced denials of care and letters demanding they return to veterans hospitals. Some said they have waited months or years for the VA to set up or renew appointments with private doctors.
Warner Springs resident John Seymour, who lives an hour and a half from the closest VA facility, has waited two years for the VA to arrange a treatment plan for his debilitating illness.
Seymour suffers from a plethora of conditions that are commonplace among America’s veterans, including PTSD, diabetes and severe spinal injury. He has also developed non-epileptic seizures from psychological distress, which cause uncontrollable spasms and leave him unable to communicate.
A VA neurologist diagnosed Seymour’s seizures about two years ago and recommended he try cognitive behavioral therapy, but the doctor didn’t submit a treatment request.
Over time, Seymour’s symptoms grew more extreme. He collapsed in the bathtub, unable to breathe, and in a similar incident, ended up in the emergency room. He waited months for another neurology appointment, which was cancelled twice.
In March, the veteran’s VA primary care doctor offered to send in a treatment request, which was routed to the VA Office of Community Care. It’s still pending.
Amy Warix, the veteran’s wife and full-time caregiver, said the VA has taken so long on the request that staff couldn’t find it in their computer system. Warix had to call her husband’s doctor and have the request resubmitted.


Now, when she asks for updates, Warix gleans little information.
"They can’t say, ‘No, you don’t get the care,’ and they can’t say, ‘Yes, you will get the care,’” she said. “They’ll just say, ‘It is processing.’”
Warix spends hours on the phone with the VA trying to manage incomplete medical requests.
She spent seven months asking the VA to restart visits with a private psychologist when they were suddenly cut off in November — just after her husband had shared thoughts of suicide. She is still waiting for the VA to approve more appointments with a neighborhood dentist to finish urgent work that began in March.
“He’s a patient that needs continuous care,” Warix said. “So I always have a referral that I am chasing down because they haven’t finished processing yet.”


Since the Mission Act launched, the VA decided to handle outsourced health care requests itself — taking over the job from its contractors — so its employees could have direct contact with veterans about their needs. But the department was critically understaffed and unable to handle the workload, according to federal reports from the Government Accountability Office.
The staffing shortage has impacted veterans seeking medical care. In mid-2020, patients were waiting an average of three weeks for the VA to process specialty care requests and six weeks until their community appointments. By comparison, referrals from one VA doctor to another took one week.
National spokespeople said veterans with urgent needs are prioritized, and processing time for non-VA treatments is now under two days.
Lawmakers have sent numerous inquiries to the VA asking why veterans in their districts are facing long waits for community care. In June, 10 Congress people from Washington told the department that their constituents were waiting two months for the VA to arrange health care visits and receiving little communication about the delays.
“We request your immediate action to resolve these issues and improve access to care,” the letter said.
Washington representative Dan Newhouse, who co-authored the letter, said veterans account for roughly half of the calls he receives from residents in his rural district. The VA never responded to the concerns he and his colleagues raised.
“This is an effort to get closer to perfection on something that I think overall has been a big improvement, but can be better,” Newhouse said. “We all want to do better for our veterans.”
Congress people from both political parties said the VA does a good job delivering health care, and pointed out that many of their constituents love the medical services they receive. A VA survey shows 90% of patients would recommend the health care system to another veteran.
The VA performs as well as private hospitals on measures of quality, including cancer screenings and blood pressure control. Compared to civilians in the private sector, veterans face shorter wait times to see VA doctors.
But like in every hospital system, some patients will need treatment the VA can’t provide.
The federal department dates back more than a century and has its roots in the Revolutionary War. For decades, the VA has purchased private care to help ailing veterans.
“In most medical centers, there’s something they’re going to have to refer you out for at some point,” said Gallucci from VFW. “It’s unrealistic to think that VA can provide everything.”
Gallucci served eight years in the U.S. Army Reserve and was deployed to Iraq in 2003. Now, he helps other former service members access benefits through the VA.
“It’s not a question of, ‘Is VA care or community care better?’" Gallucci said. “It’s about how do these systems complement each other, how do they work to effectively deliver care that veterans need?”
WATCH RELATED: Why the VA is stopping doctors from sending veterans to other hospitals